|
|
Bladder Rupture
Intraperitoneal and Extraperitoneal
General Considerations
- Can be secondary to traumatic or iatrogenic injury
- Five types of rupture
- Type I: Bladder contusion
- Most common form
- Results from incomplete tear of bladder mucosa
- Cystography is normal
- Type II: Intraperitoneal rupture
- Results from trauma to lower abdomen when bladder is distended
- Because bladder dome is weakest portion, it ruptures most easily
- Contrast is then seen in the paracolic gutters and between
loops of small bowel
- Type III: Interstitial injury-rare
- Caused by a tear of the serosal surface
- Mural defect without extravasation will be seen
- Type IV: Extraperitoneal
- Almost always associated with pelvic fractures
- Usually close to base of bladder anterolaterally
- Subdivided into
- Simple, with extraluminal contrast limited to perivesical space
- Complex, with extraluminal contrast extending to thigh,
scrotum or perineum
- Type V: Combined extra- and intraperitoneal rupture
- Extraperitoneal bladder rupture is the most common type
- Occurs in 80% of bladder rupture cases.
- Extraperitoneal bladder rupture generally secondary to adjacent pelvic fracture or an avulsion tear at fixation points of puboprostatic ligaments
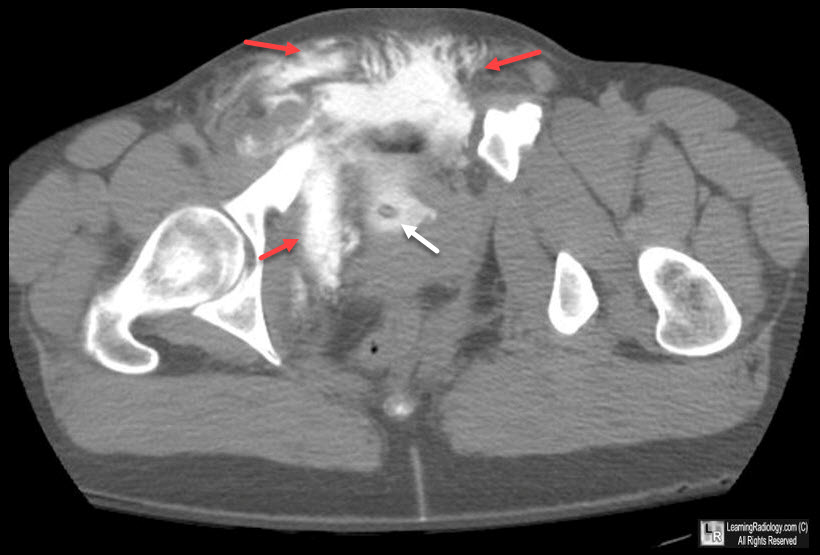
Extraperitoneal Bladder Rupture. CT of the pelvis following contrast shows a Foley catheter (white arrow) in the
lumen of the urinary bladder with ladder in the extraperitoneal spaces (red arrows).
- Intraperitoneal bladder rupture
- Usually iatrogenic or secondary to penetrating injury
- Blunt trauma more likely to result in intraperitoneal rupture in children
than in adults
- Because the pediatric bladder is more intraperitoneal in location.
- The adult bladder dome remains mostly extraperitoneal
- Blunt trauma in an adult can result in intraperitoneal rupture
only if the bladder is fully distended
- Imaging findings
- Extraluminal contrast extends into paracolic gutters
- Contrast outlines loops of bowel
- While extraperitoneal bladder rupture can be treated conservatively, intraperitoneal bladder rupture requires surgical repair
- Highest morbidity and rupture mortality is associated with
intraperitoneal rupture because of potential for development of chemical peritonitis
Imaging findings
- Diagnostic evaluation of bladder rupture includes voiding cystourethrography (VCUG) or CT scan
- VCUG
- Voiding cystourethrography historically been preferred contrast enhanced study for diagnosis of bladder rupture
- Bladder needs to be fully distended and evaluation of a
post-voiding film essential
- Plain film:
- "Pear-shaped" bladder
- Paralytic ileus
- Upward displacement of ileal loops
- Flame-shaped contrast extravasation into perivesical fat
- Best seen on postvoid films
- May extend into thigh / anterior abdominal wall
- US
- "Bladder within a bladder" = bladder surrounded by fluid collection

Bladder Rupture, Extraperitoneal. One image from an IVU shows a flame-shaped density adjacent to
right lateral wall of bladder representing extra-peritoneal contrast
from a bladder rupture
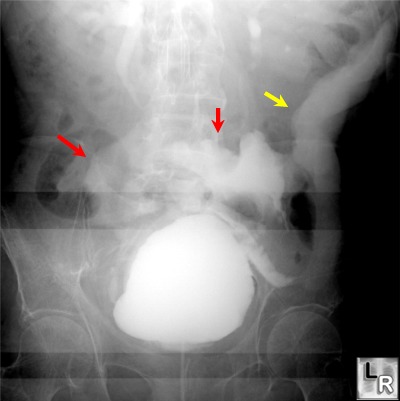
Intraperitoneal
bladder
rupture. Note
the
extraluminal
contrast
(red
arrows)
outside
the
confines
of the
normal
bladder
and
spreading
into
the
peritoneal
cavity.
There
is
contrast
in the
left
paracolic
gutter
(yellow
arrow),
not
within
the
bowel.
The
intrarenal
collecting
systems
and
ureters
are
visualized
because
the
patient
had a
contrast
enhanced
CT
done
moments
earlier.
Amersham Health Encyclopedia
|
|
|