|
Idiopathic Pulmonary Hemorrhage and Goodpasture's Syndrome
IPH
•
Both are characterized by repeated episodes of pulmonary hemorrhage
•
Both produce iron-deficiency anemia and both can produce pulmonary
insufficiency
• Pathology
• Hemorrhage is typically confined to peripheral airspaces
• Diffuse interstitial fibrosis, hemosiderosis are common
• Vasculitis doesn't always occur even though these are autoimmune
diseases
•
Hemoptysis more copious in IPH
•
Prognosis for both diseases is grave – both are treated with steroids and
cytotoxic agents
Idiopathic
pulmonary hemorrhage
•
Occurs most commonly in children under the age of ten
•
When it occurs in adults, it is twice as common in men
•
Anti-glomerular basement membrane antibody should be absent (unlike
Goodpasture’s)
Goodpasture’s
syndrome
•
Goodpasture’s includes renal disease
•
Renal lesion is glomerulonephritis
•
It is a disease of young adults
•
Most are men
•
Autoimmune etiology
•
Both lung and renal pathology believed 2° to anti-glomerular basement
membrane antibody cross reacting with lung basement membrane
Imaging Findings
•
Identical changes in both diseases
•
Early in the disease, it is alveolar in nature, more prominent at the bases
and perihilar regions — simulates pulmonary edema
•
Within 2-3 days, the blood is absorbed in to the interstitium and the pattern
changes to interstitial reticular
•
By about 10 days, the reticular disease disappears
•
With repeated bleeds, there is hemosiderin deposit in the lungs and
progressive pulmonary fibrosis occurs
•
Once this occurs, the new hemorrhage is superimposed on the old interstitial
disease, so the reticular pattern
remains rather than disappears when the blood is absorbed
•
May have pulmonary hypertension
•
May have hilar adenopathy
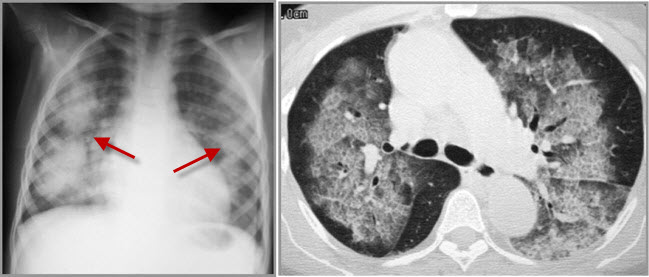
Goodpasture Syndrome. There is bilateral central airspace disease seen on both chest radiograph (red arrows) and axial CT scan of the lung. This could represent pulmonary edema, pneumonia, aspiration or hemorrhage. The patient had known glomerulonephritis and hemoptysis.
|