|
|
Pericardial Calcifications
Constrictive Pericarditis
- Calcification in the pericardium is most likely
inflammatory in nature
- Can be seen with a variety of infections,
trauma, and neoplasms
- Calcification most commonly occurs along the
inferior diaphragmatic surface of the pericardium surrounding the
ventricles
- Thin, egg-shell like calcification is more often
associated with viral infection or uremia
- Calcification from old TB is often thick,
confluent, and irregular in appearance, especially when compared with
myocardial calcification
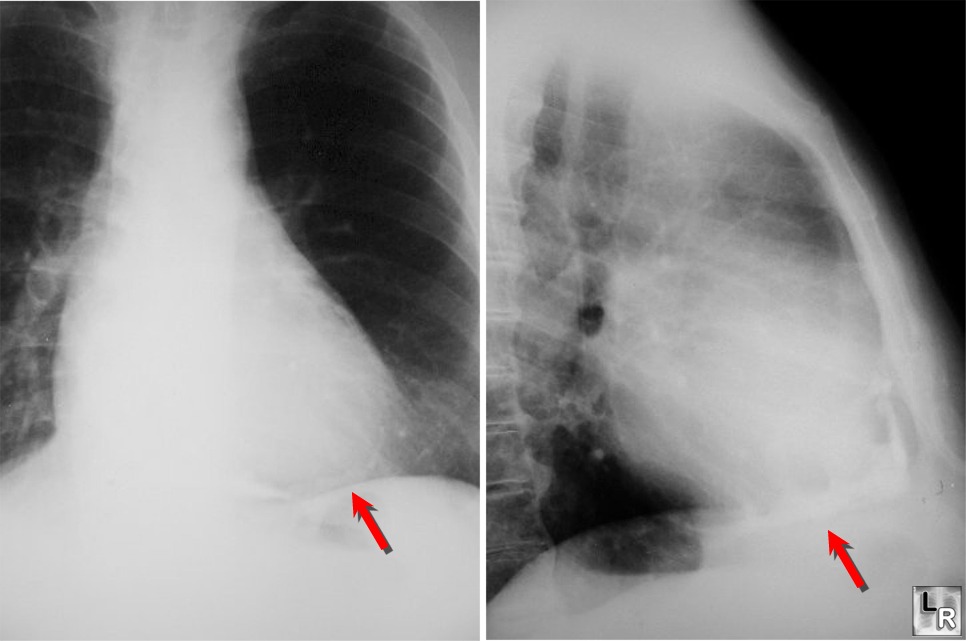
PA and
lateral close-ups show thick pericardial calcification around
apex of heart from patient with history of tuberculous pericarditis
- Calcification is seen in 1/3-1/2 of patients with
constrictive pericarditis
- Its presence does not imply constriction
- Pericardial calcification must be differentiated
from coronary artery calcification, valvular calcification, calcified
myocardial infarct or ventricular aneurysm, left atrial calcification,
or calcification outside the heart
- This can usually be accomplished by the
locations of these calcifications on multiple views, or the
radiographic appearance of the calcium
- Constrictive Pericarditis
- Present when a fibrotic, thickened, and adherent
pericardium restricts diastolic filling of the heart.
- Usually begins with an initial episode of acute
pericarditis
- May not be detected clinically
- This slowly progresses to a chronic stage
consisting of fibrous scarring and thickening of the pericardium with
obliteration of the pericardial space
- This produces uniform restriction of the filling
of all heart chambers
- Signs and Symptoms
- Reduced cardiac output ( fatigue, hypotension,
reflex tachycardia )
- Elevated systemic venous pressure ( jugular
venous distension, hepatomegaly with marked ascites and peripheral
edema )
- Pulmonary venous congestion ( exertional
dyspnea, cough and orthopnea )
- Chest pain typical of angina may be related to underperfusion of the coronary arteries or
compression of an epicardial coronary
artery by the thickened pericardium.
- Most impressive physical findings are often the
insidious development of ascites or hepatomegaly and ascites; such
patients are often mistakenly thought to suffer from hepatic cirrhosis
or an intra-abdominal tumor.
· Calcification of
the pericardium is detected in up to 50 % of patients
· This finding is
not specific for constrictive pericarditis
o A calcified
pericardium is not necessarily a constricted one
o Lateral chest
film is useful for its detection in the atrioventricular groove or along
the anterior and diaphragmatic surfaces of the right ventricle.
o Pleural effusions
are present in about 60 % of patients
§ Persistent
unexplained pleural effusions can be the presenting manifestation
· CT or MRI are
superior in the assessment of pericardial anatomy and thickness
· The diagnosis is
confirmed by cardiac catheterization
· Treatment for
constrictive pericarditis is complete resection of the pericardium
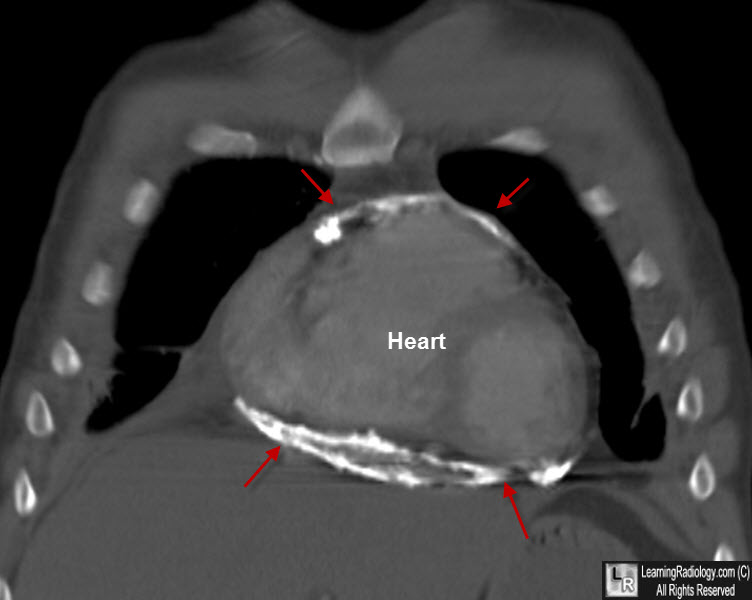
Constrictive Pericarditis. Coronal re-formatted CT of chest shows markedly thick pericardial calcification around
the heart from patient with history of tuberculous pericarditis
Acknowledgement to Eduardo Benchimol Saad, MD
|
|
|