
Ultrasound and CorrelativeImaging of Renal TransplantsMarch, 2012
Mindy M. Horrow, MD, FACR, FSRU, FAIUM
Director of Body Imaging
Einstein Medical Center, Philadelphia, PA
Professor of Radiology
Thomas Jefferson University

Outline
•Introduction
•Normal gray scale and Doppler evaluation
•Collections
•Infections
•Vascular Complications: Renal Artery, RenalVein, AVF, PSA
•Other: tumors, calcifications, hernias,miscellaneous
•Pitfalls and Bonus Cases

Clinical Perspective
•Most effective primary treatment of CRF
•Anticipated graft survival of 90 – 95%
–New generation immunosuppressives (cyclosporin,tacrolilmus) reduce T-cell activation, improving graftsurvival by almost eliminating acute rejection
•Demand for renal transplants greater thansupply
–Extended donor supply with older kidneys, multiplerenal arteries, etc.
★ Greater imaging challenges ★
Cosgrove D, Chan K. USQ 2008;24:77-87

Surgical Technique
•Vascular supply from end-to-sideanastomosis of donor artery and vein toexternal iliac artery and vein. If multiplearteries, usually joined with singleanastomosis to EIA
•Ureter anastomosed to superolateral wall ofurinary bladder
•En bloc transplant of a set or pediatrickidneys with caudal ends of IVC and Aortaanastomosed end-to-side to recipient's EIAand EIV, or with separate anastomoses
•Usually extraperitoneal, right side preferred

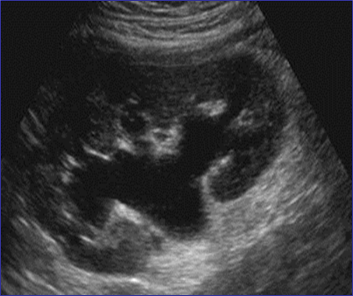
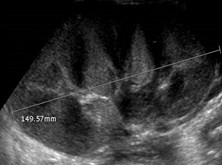
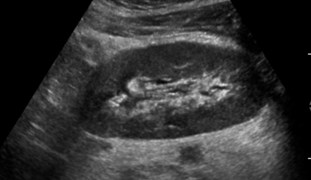
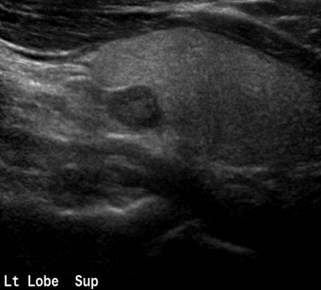
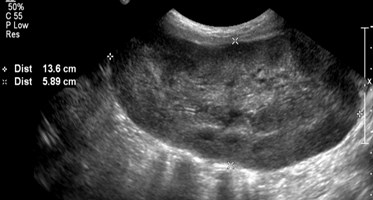
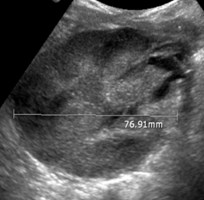
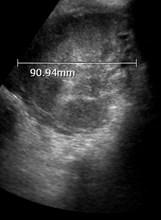
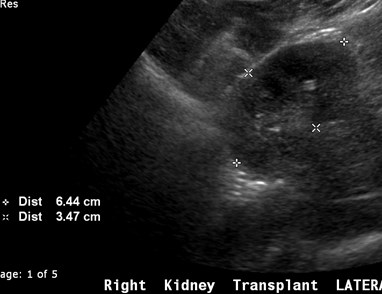
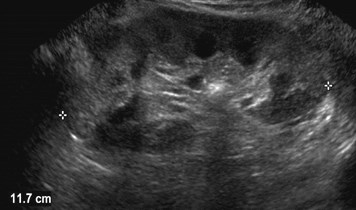
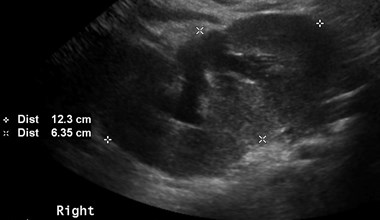
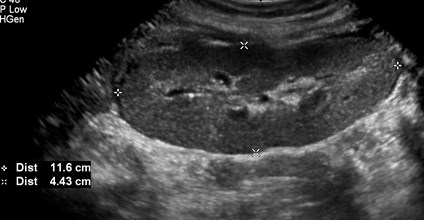
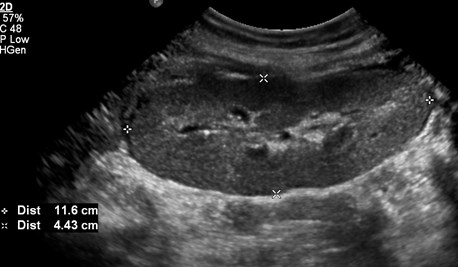
Grey Scale Evaluation
•Usually parallel to incision with hiluminferiorly and posteriorly
•Obtain longitudinal and transversemeasurements. Usually hypertrophies~ 15% in first 2 weeks and mayincrease by 40% in first 6 months.
Absy. Br J Radiol 1987;60:525

Grey Scale Evaluation
•Because kidney is more superficial,pyramids are more easily visualized,accentuating the cortico-medullarydifferentiation.
•Evaluate for any intrinsic pathology:calculi, tumors, etc.
•Collections, hydronephrosis, urothelialthickening

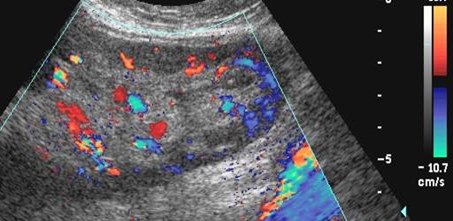
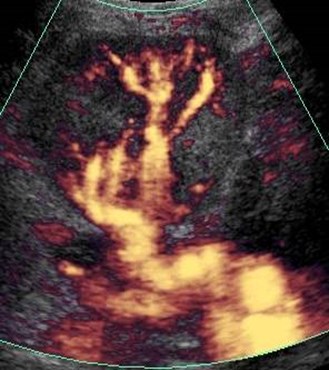
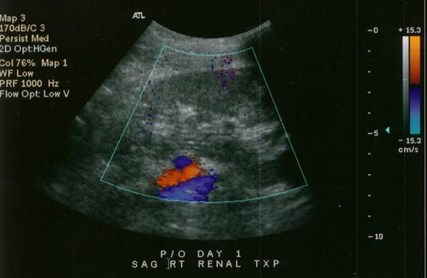
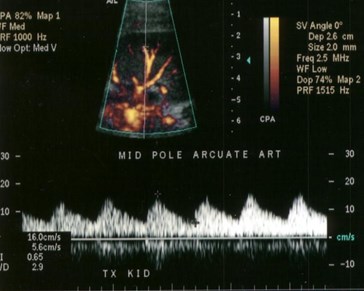
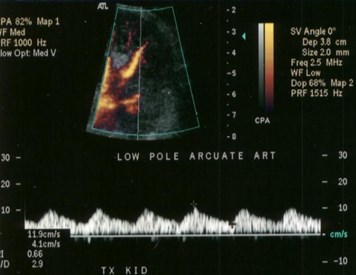
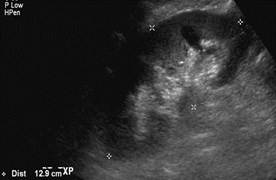
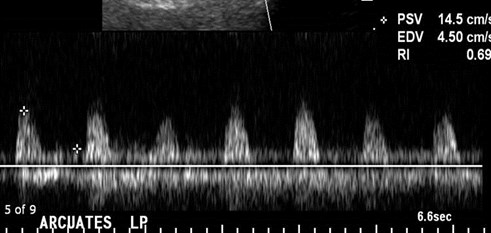
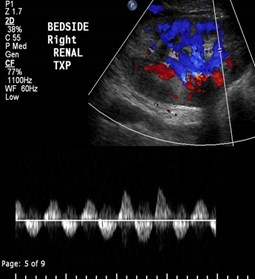
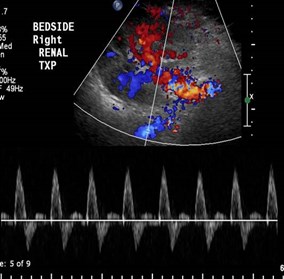
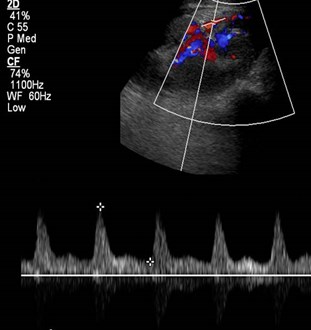
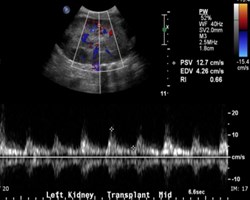
Doppler Evaluation
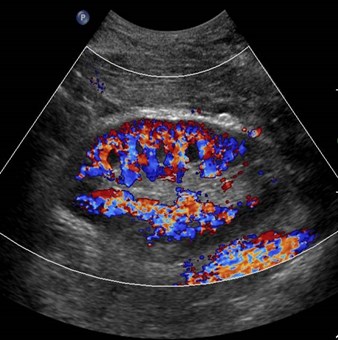
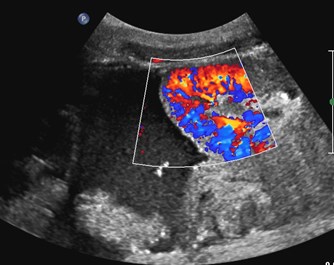
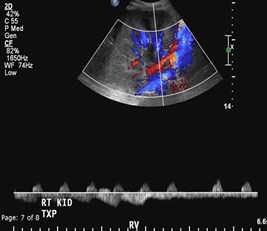
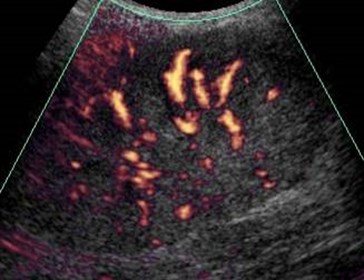
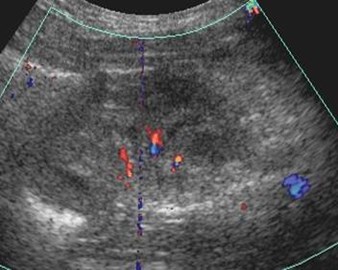
•Screen and image with color/power Doppler,looking for focal and/or diffusehypoperfusion.
•Obtain spectral traces of arcuate orinterlobar arteries in upper, mid and lowerpoles with appropriate factors.
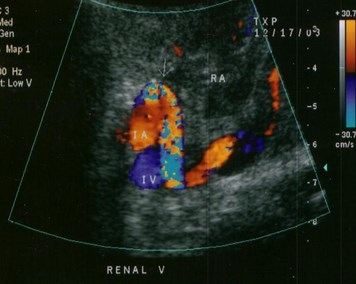
•Image and obtain spectral Doppler of mainrenal artery and vein and external iliac arteryand vein with attention to anastomoses


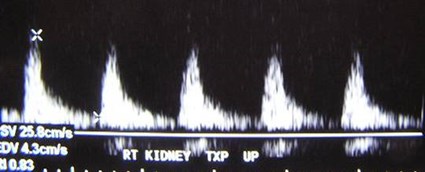
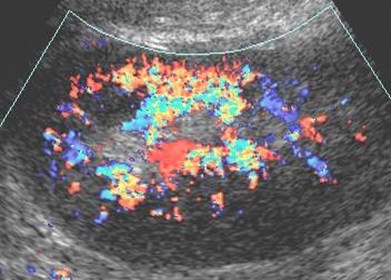
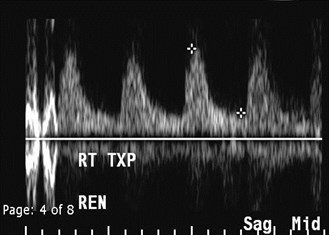
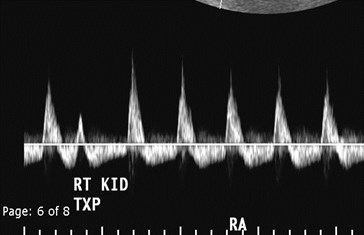
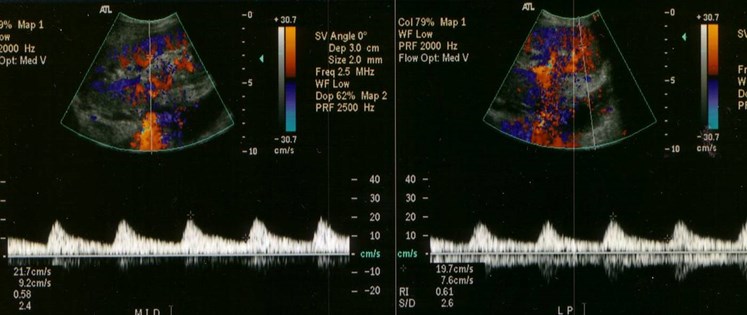
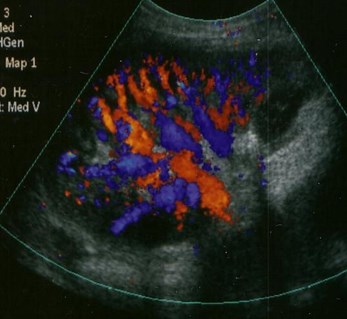
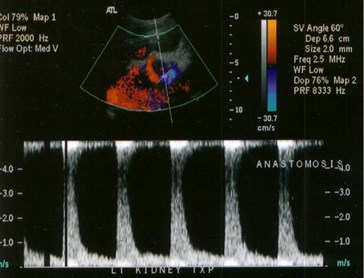
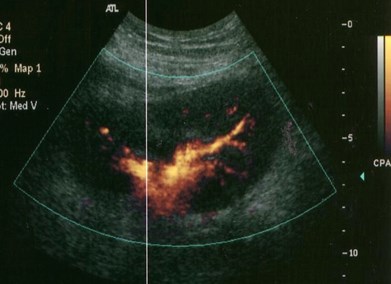
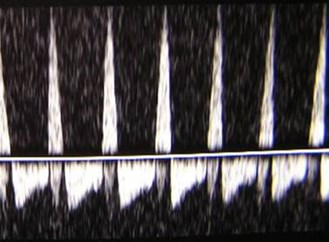
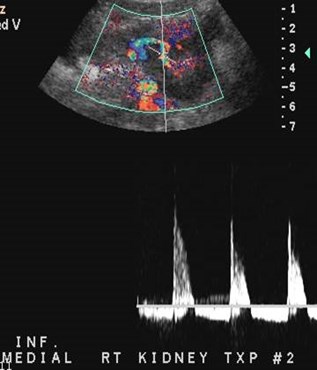
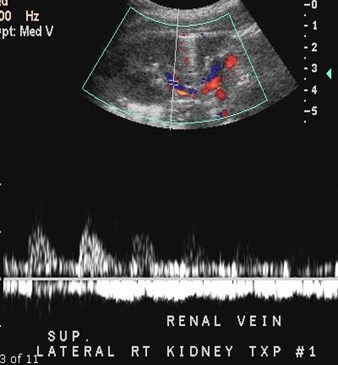
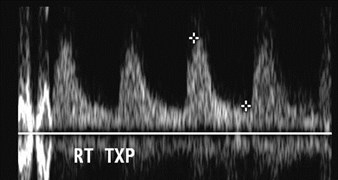
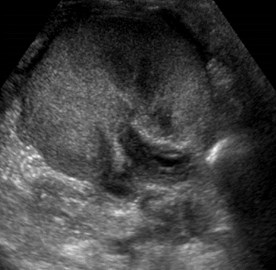
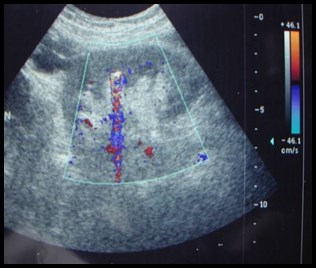
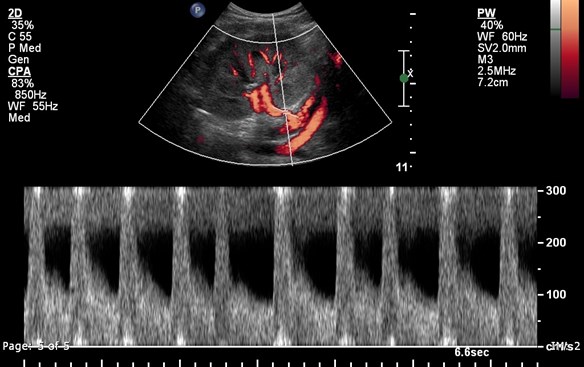
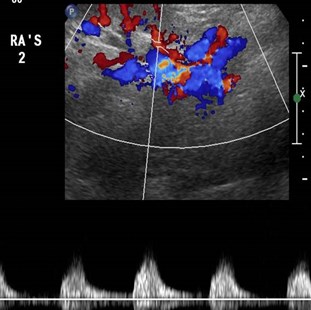
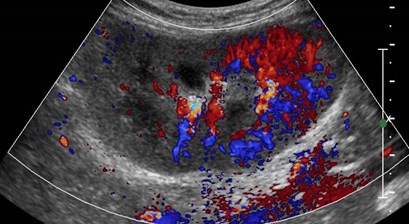
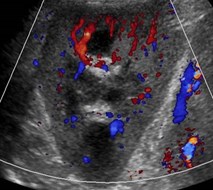
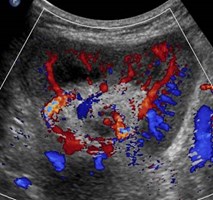
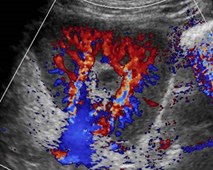
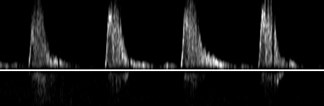
Normal color andspectral Doppler


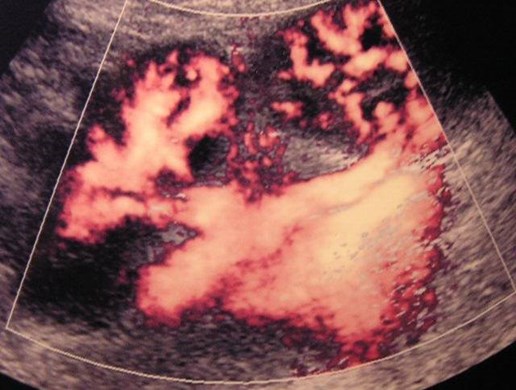
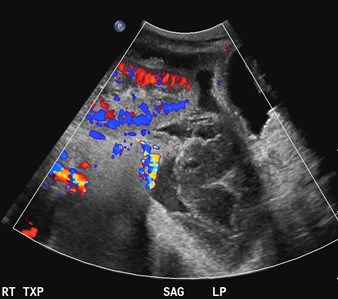
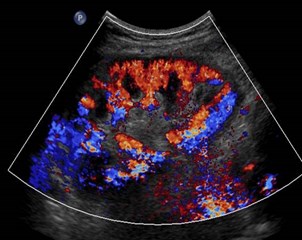
Normal power Doppler of en bloc pediatrickidney transplants

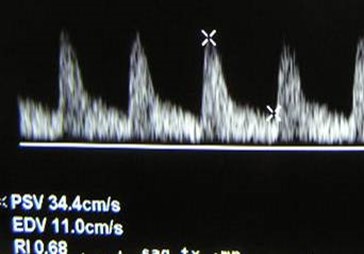
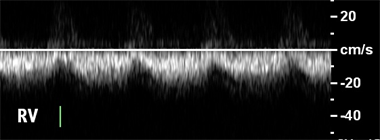
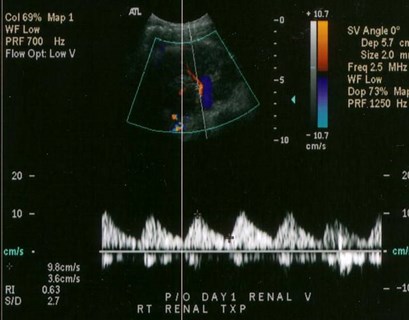
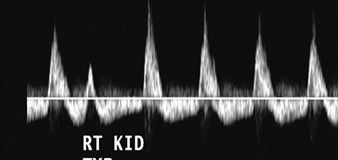
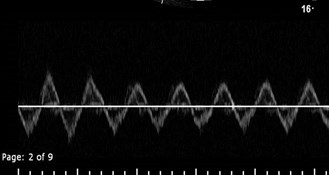
Normal Doppler Findings
•Arteries- brisk upstroke, low resistance withnormal resistive index of 0.6 to 0.8.
–Resistive Index= (Peak systole – End Diastole) / Peak Systole
•Normal velocity main renal artery < 200cm/sec, RA/EIA velocity ration < 2
•Veins- may be monophasic with continuousflow or demonstrate some pulsatility withcardiac cycle.

Hydronephrosis
•Obstruction is rare,though will usually beat UV junction fromstricture or intra-luminal lesion.
•Mild dilatation may be2º increased urinevolume of sole kidney,decreased ureterictone, U-V reflux



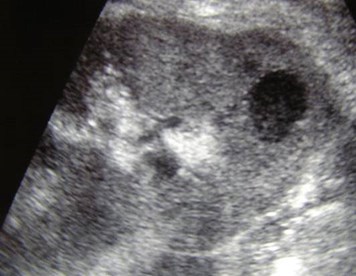
Lymphocele



Lymphocele with some pressure effect on kidney

Day One after transplant
Superficial hematoma notappreciated on US




Inferior to kidney
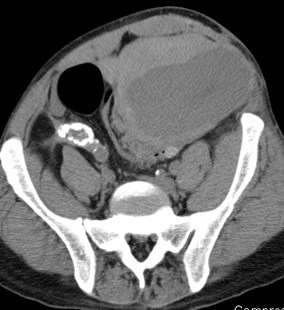
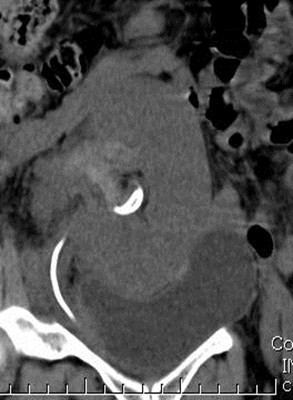
Hydronephrosis secondary to stenoticureter with associated urinoma


Intraperitoneal Transplant
Hemoperitoneum

Gas containing peri-renal abscess

Initial imaging
Imaging 1 day post biopsy


Subcapsular hematoma causingelevated resistive index

Fluid Collections
•Post- operative hematomas- appearancedepends upon chronicity.
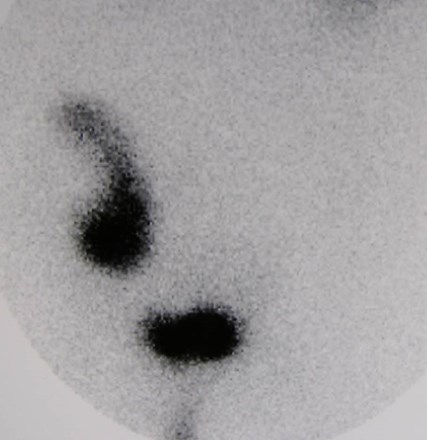
•Urine leaks or urinomas- due to anastomoticleaks or ureteric ischemia. Appear well defined,anechoic with occasional hydronephrosis. Mayuse radionuclide imaging to confirm nature ofcollection
•Lymphoceles- occur 4 – 8 weeks after surgeryin 15%. May obstruct ureter or veins. Appearwell defined and either anechoic or with fineseptations.
Brown. Radiographics 2000;20:607
Park, etal. JUM 2007;26:615-633

Parenchymal Pathology
•Acute Tubular Necrosis
•Rejection
•Drug Nephrotoxicity

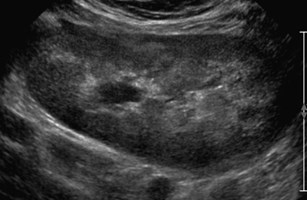
Acute Tubular Necrosis
•Occurs to some extent in all cadaverictransplants
•Most common cause of delayed graft function(need for dialysis in 2 weeks post transplant)
•Non-specific imaging features: normal orchanges in echogenicity, qualitativelydecreased color flow, RI may be normal orincreased.

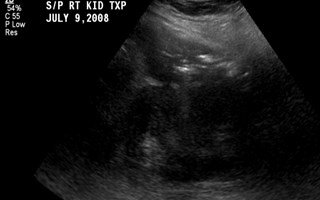
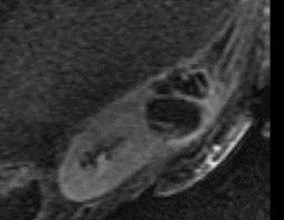
Acute Tubular Necrosis, 6 days aftertransplant

Rejection
•Hyperacute- rarely imaged since itoccurs during surgery
•Acute- occurs in up to 40% in first fewweeks and is a poor long termprognostic indicator.
•Similar US and radionuclide findings
•US findings non-specific


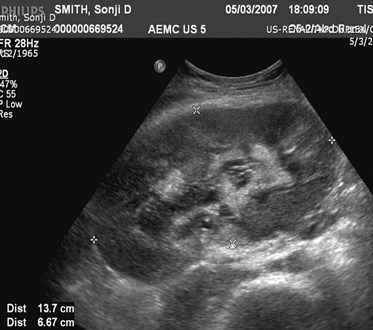
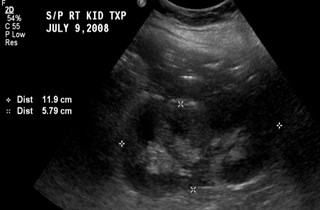
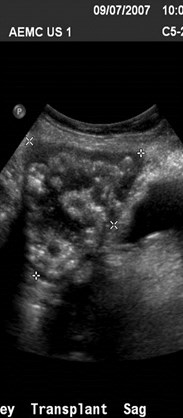
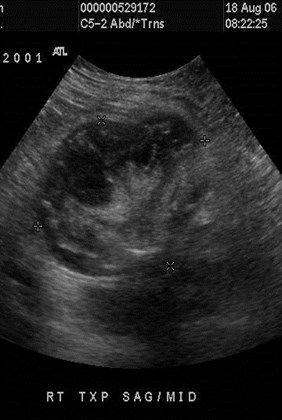
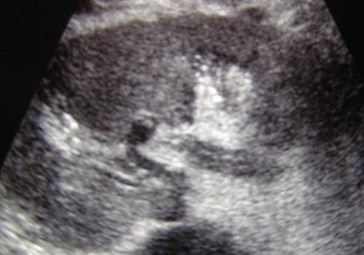
Increased size and urothelial thickening:Acute on Chronic Rejection


Patient on dialysis, anti-rejectionmedications withheld

Severely enlarged, painful kidneywith marked urothelial thickening,required nephrectomy
(has potential for rupture)


9-07
11-07
Baseline imaging Repeat because of rising creatinine

11-07
9-07
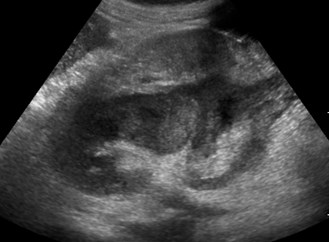
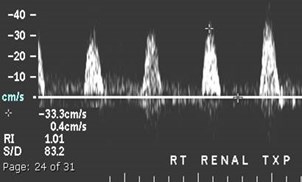
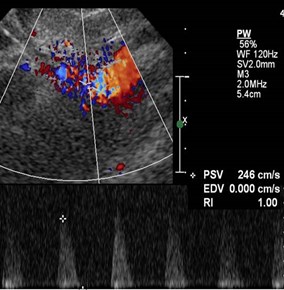
Acute Rejection: reversed diastolic flow,urothelial thickening, marked enlargement

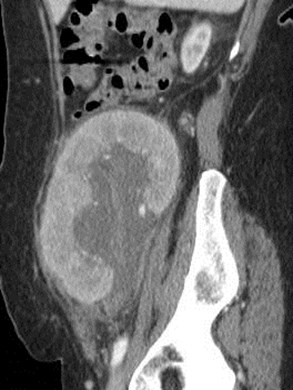
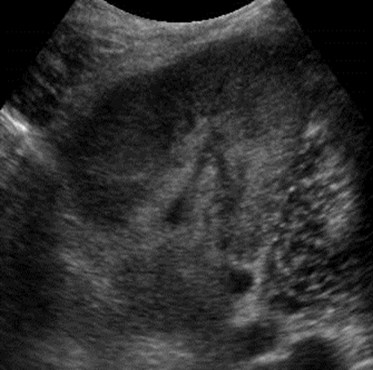
Chronic Rejection
•Most common cause of late graft loss.
•Progressive loss of renal functionbeginning 3 months after transplant.Patients with acute rejection arepredisposed.
•US- Cortical thinning, mildhydronephrosis, prominent sinus fat,dystrophic calcifications, decreasedcolor, normal or increased RI.

Chronic Rejection

Chronic Rejection:progressive nephrocalcinosis

Infections
•Pyelonephritis
•Pyonephrosis
•Abscess


5 years after transplant with vomiting,dehydration and elevated creatinine



Pyelonephritis

Swelling over region of one week oldtransplant with elevated creatinine



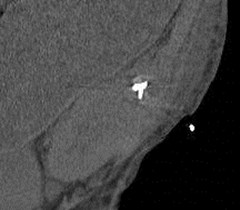
Emphysematous Pyelonephritis




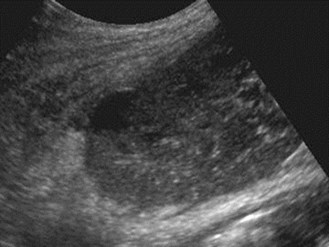
Pyonephrosis



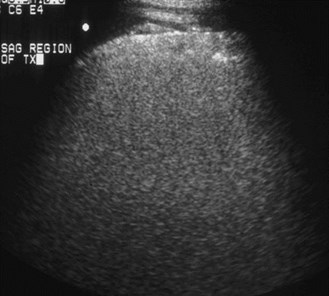
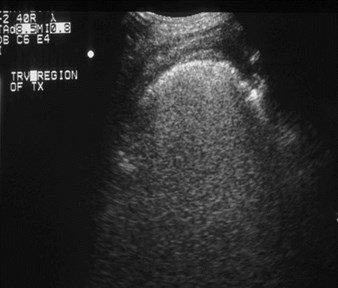
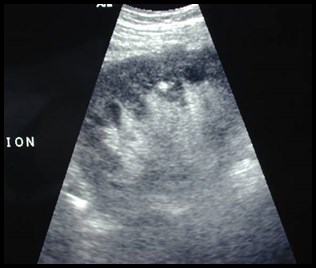
Patient with fever,imaging with 5-2MHz transducer


Imaging with 7-4 MHztransducer
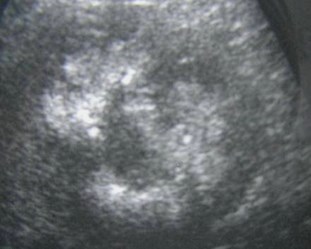
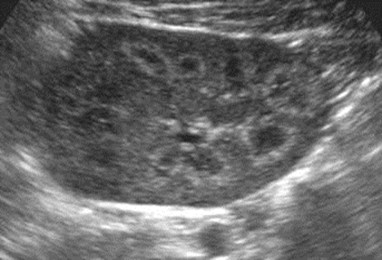
MultipleAbscesses

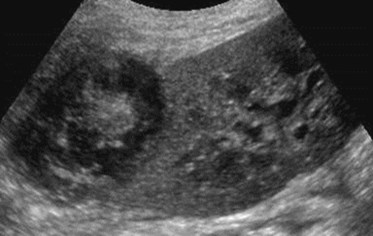
June
July
T2 with gadolinium
Renal Abscess drained percutaneously

Vascular Complications
•Renal Artery: thrombosis, stenosis, kink,pseudoaneurysm, arteriovenous fistula
•Renal Vein: thrombosis, stenosis
•Infarct
•“Steal phenomenon”



Immediatepost operativeUS

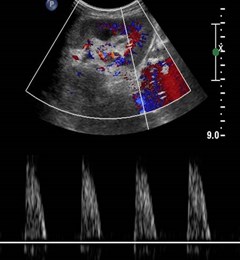
Renal Artery Thrombosis

Renal Artery Thrombosis
•Occurs in < 1% typically within first month.
•Most common cause is acute rejection withretrograde thrombosis of small to largearteries.
•Other causes: pediatric kidneys, emboli,acquired stenosis, hypotension, vascularkink, hypercoagulable state, pooranastomosis, trauma
•US: Absent arterial and venous flow inkidney and main renal artery.



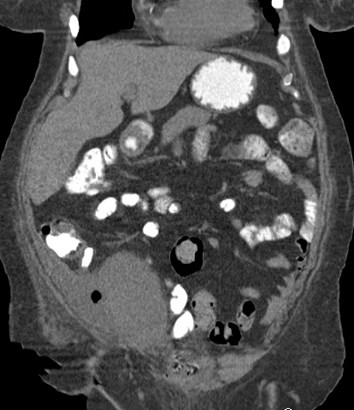
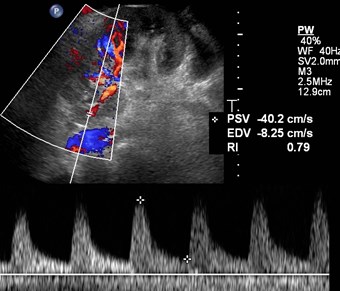
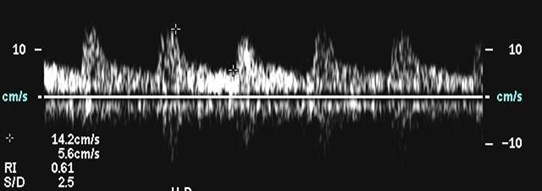
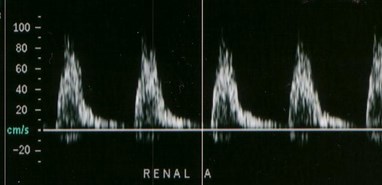
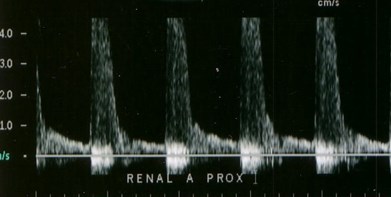
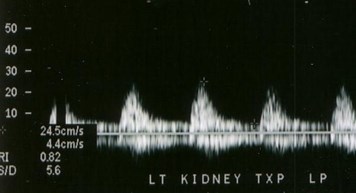
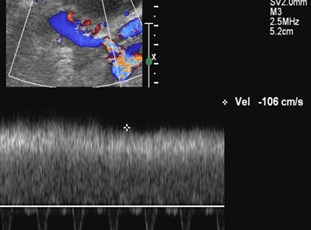
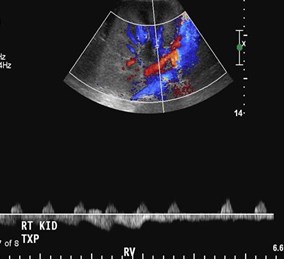
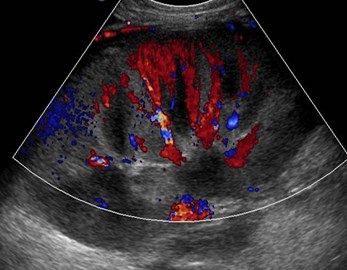
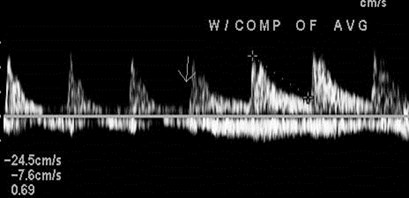
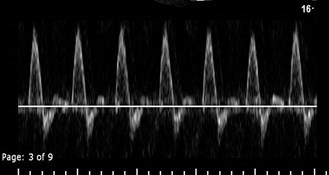
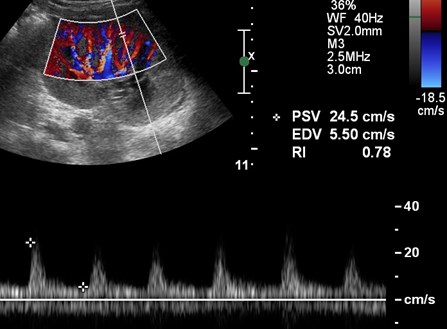
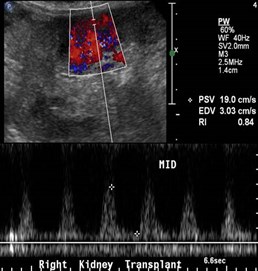
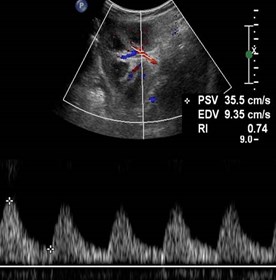
Parvus-tardus waveforms in arcuate arteries



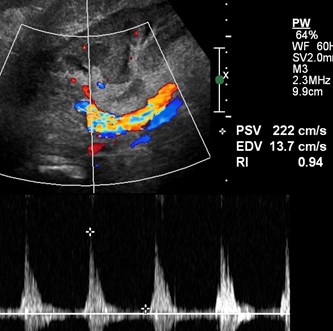
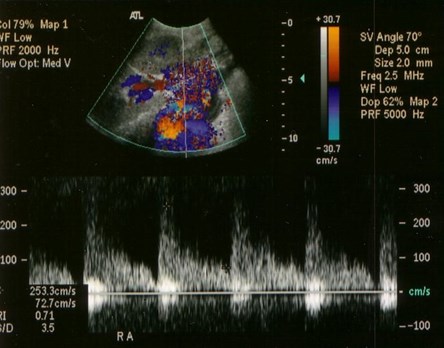
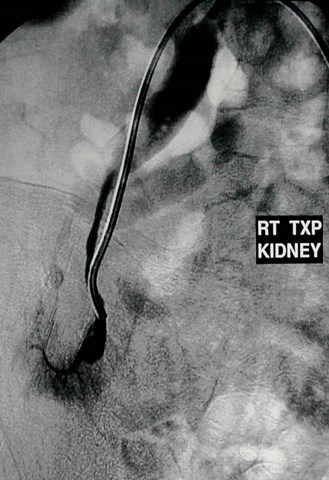
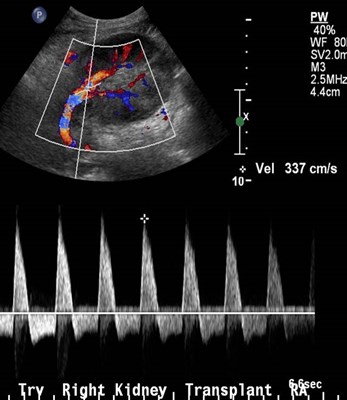
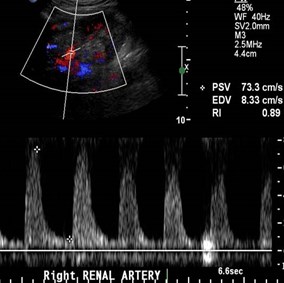
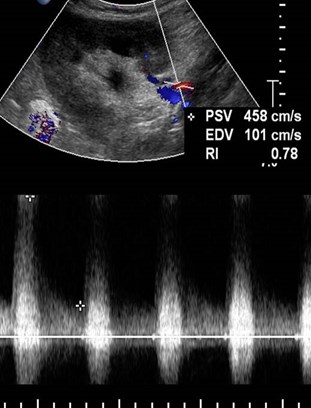
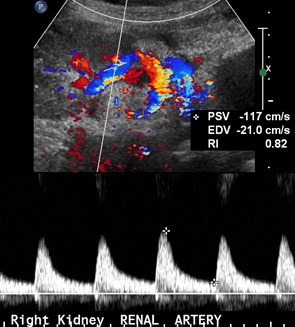
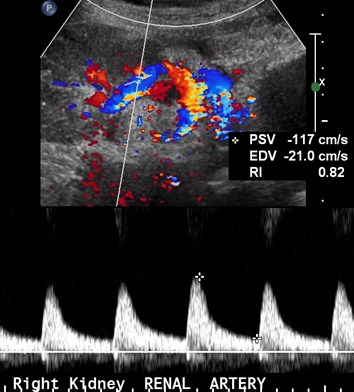
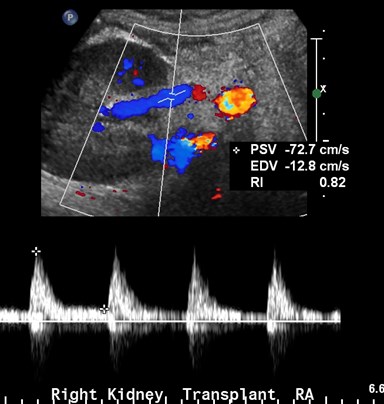
Renal Artery Stenosis
•Most common vascular complication in up to10% in first year.
•Three possible sites:
–Donor portion, typically at end-to-sideanastomosis
–Recipient portion- more uncommon, fromintraoperative clamp or intrinsic atherosclerosis
–At anastomosis- more frequent in end-to-endanastomoses

US Findings of RAS
•Parvus-tardus flow in intra-parenchymalvessels
•Use color Doppler to locate stenosis. Peaksystolic velocities > 200 cm/sec withturbulent flow.
•False positive diagnoses may occur withabrupt turn in the main renal artery.
•With chronic rejection, segmental renalartery stenoses may occur
Dodd. AJR 1991;128:1581

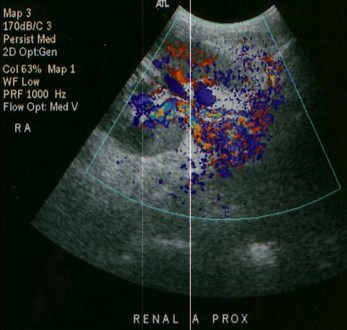

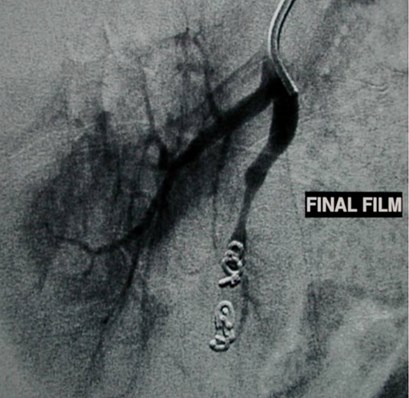
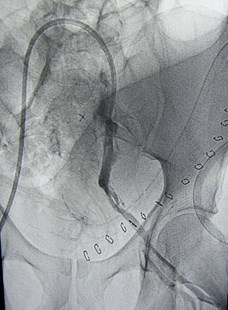
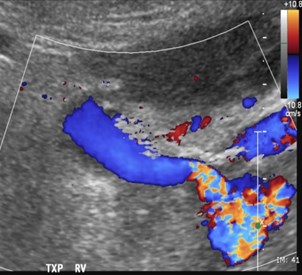
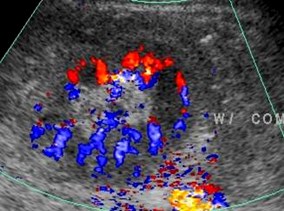
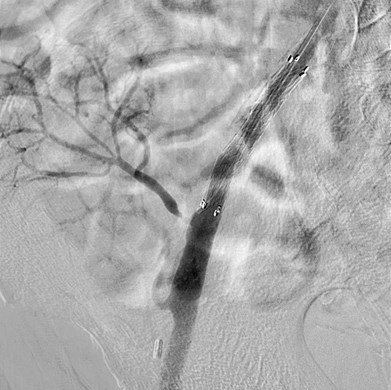
Early venous opacification impliesArteriovenous Fistula


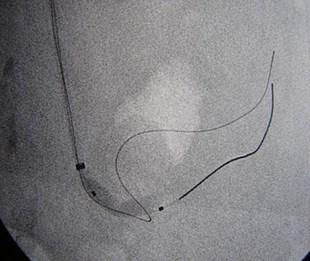

Angioplasty of stenosis reveals AVF


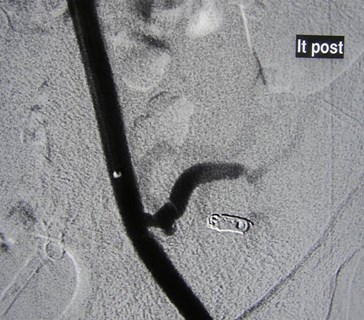
Embolization of AVF with coils
Residual renal artery stenosis

Residual stenosis,coils and small infarct

Day One afterRenal TX

Day Two



Renal Artery Kink

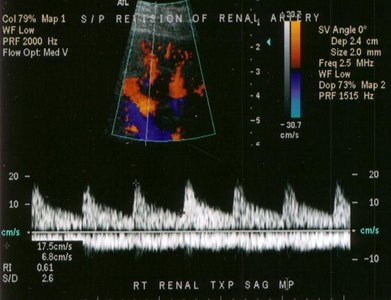
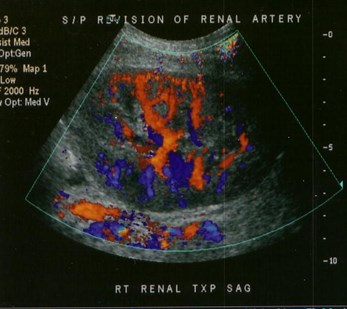
S/P revision of renal artery

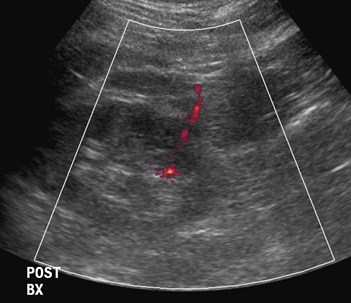
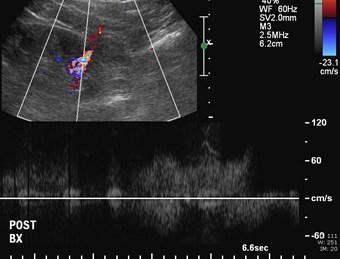

Immediately after biopsy

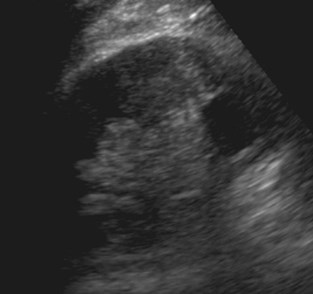
2 days later
Pseudoaneurysm


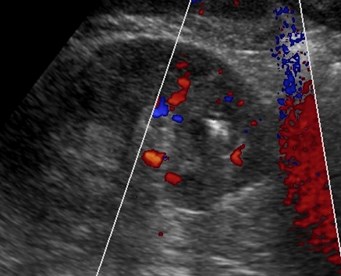
Successful coil embolization


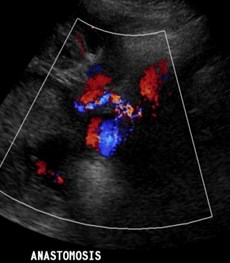
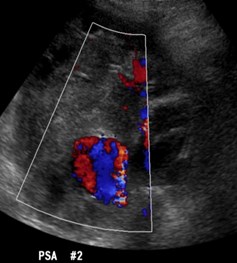
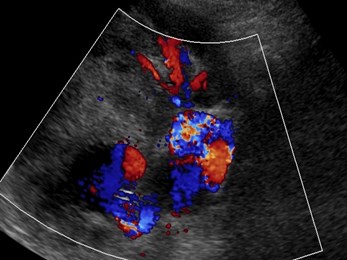
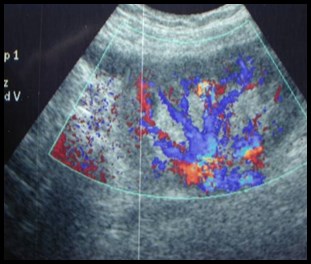
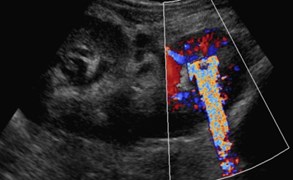
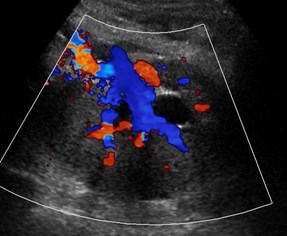
Arteriovenous fistula andPseudoaneurysm

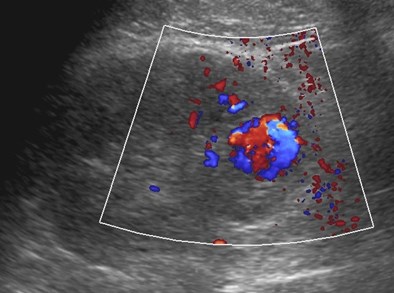
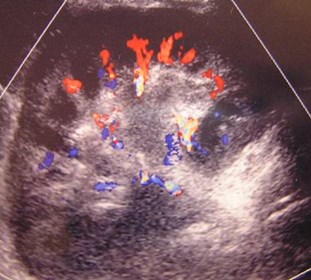
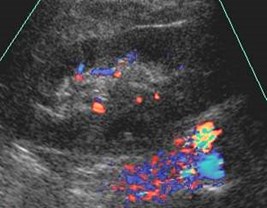
AVF and PSA
•Both are typically the result of trauma duringpercutaneous biopsy.
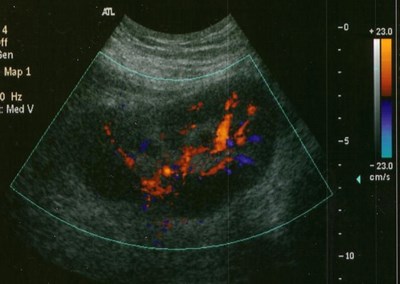
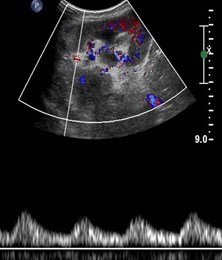
•AVF- color shows focal area of mixed colorsoccasionally with feeding vessels. AVMproduces vibrations which result in colorassigned to the perivascular tissues.
•PSA- may appear as a simple cyst on greyscale imaging but with typical swirling arterialflow on Doppler

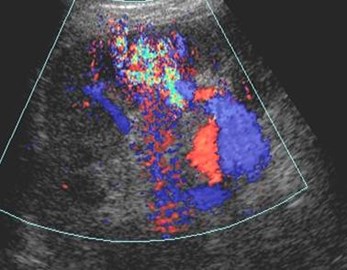
A-V Fistula

Bacteremia



Mycotic Aneurysms require stentthrombosis and sacrifice of kidney


Renal Infarct

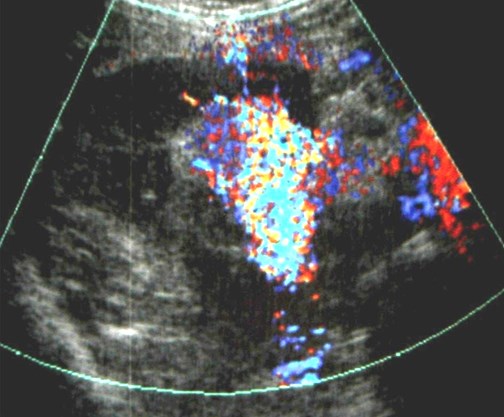
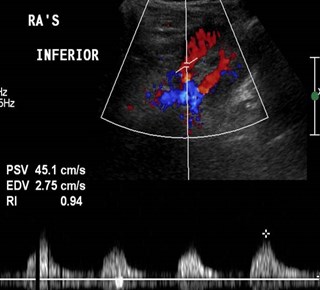
Acute Renal Vein Thrombosis


CFV w/o CFV w



Initial image #1 thrombolysis #2 thrombolysis
Renal vein thrombosis 2º stenosisof external iliac vein

Immediate post-op imaging of en-blocpediatric kidneys
Medial kidney with renalvein thrombosis


12 hours later
Lateral kidney withrenal vein thrombosis

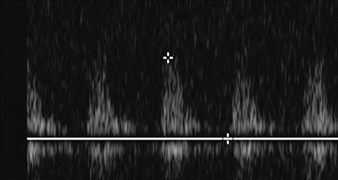
Venous Thrombosis
•Occurs in up to 4% transplants
•Sx: acute pain 2° swelling of kidney, oliguria infirst week
•Causes: surgical difficulties, hypovolemia,femoral/iliac vein thrombosis, compression bycollections
•US- absent venous flow, reversal of diastolic flowin artery. Kidney may be enlarged, hypoechoic.
;295
Kaveggia.AJR 1990;155:295
Reuther.Radiology 1989;170:557


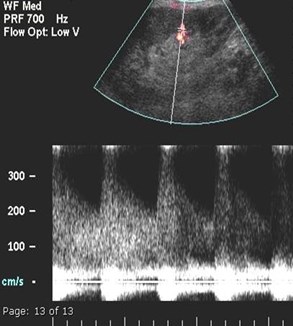
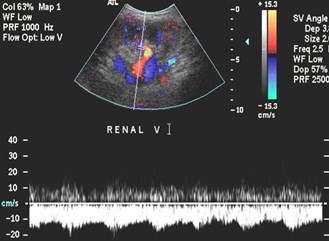
Renal Vein Stenosis
•Grey Scale- normal or hypoechoic
•Color Doppler- aliasing at stenotic site
•Spectral Doppler- 3 to 4 times increasein velocity across the region indicates ahemodynamically significant stenosis.

9-18
11-15
11-30


11-30
Other images

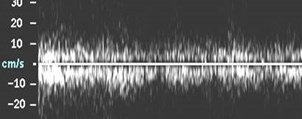
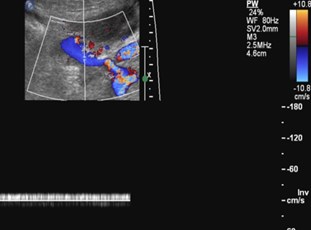
Reversed Diastolic Flow
•Though commonly ascribed to renal vein thrombosis,actually a non-specific finding
•Acute: TX < 24 hours, graft survival likely withintervention. Causes include renal vein thrombosis,hematoma, vascular kink. Since kidney lacks venouscollateral drainage, infarction occurs rapidly requiringimmediate surgery
•In more longstanding transplants causes include: ATNand rejection. These kidneys faired very poorly withhigh rate of allograft loss.
Lockhart. AJR 2008;190:650-655

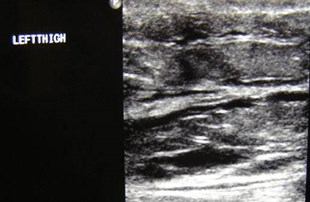
Patient with AV graft inipsilateral thigh, immediatecolor Doppler post surgery
Color Doppler duringcompression of graft
“Steal” Phenomenon
Chaudri, Horrow JUM 2006;25:939

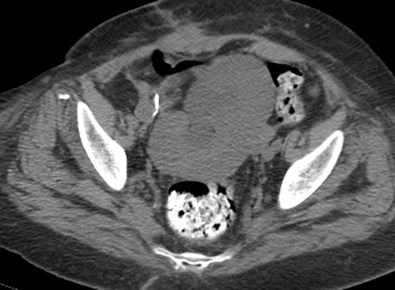
Other
•Calcifications: calculi, medullaryand cortical nephrocalcinosis
•Tumors
•Hernia
•Miscellaneous


15 years posttransplant

Medullary nephrocalcinosisand nephrolithiasis


Early medullary nephrocalcinosis



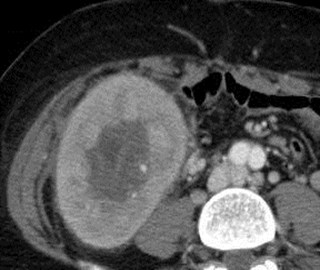
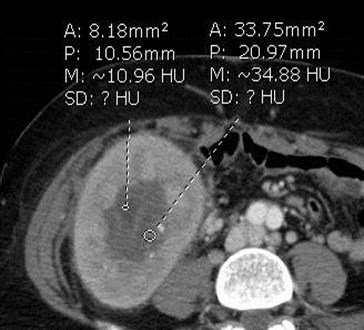
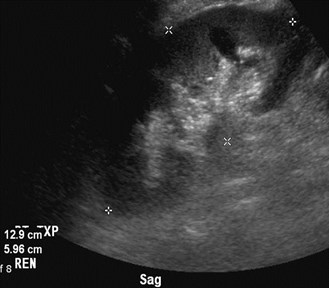
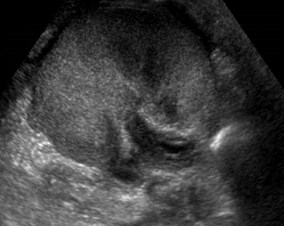
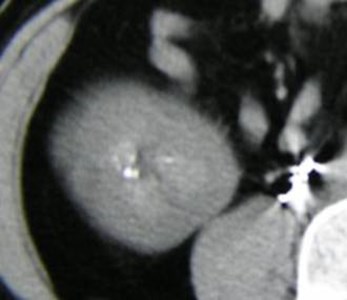
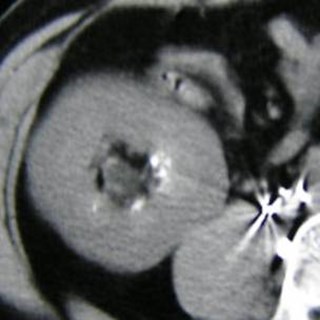
Biopsy proven renal cell carcinoma

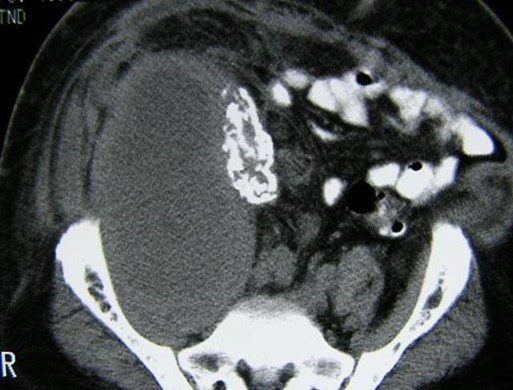
Leiomyosarcoma of failed renal transplantwith cortical nephrocalcinosis

Images of left sided kidney
from double renal
transplant


Non-contrast CT confirms left renal calculus
Also demonstrates herniation at incision

Color Doppler Twinkling Artifact
•Described in 1996 by Rahmouni as an artifact ofalternating red and blue behind certainstationary objects.Spectral Doppler of artifact generates aheterogeneous broadband signal that appears toalias.Mainly associated with nephrolithiasisSpeculation that it is generated by roughsurfaces with multiple reflectors splitting beaminto components
Rahmouni, etal Radiology 1996;199:269

5-16

8-31

Hypercalcemic secondary to hyperparathyroidismwith early calculus formation requiringparathyroidectomy and medical therapy




Calcification of urothelium



Pain over transplant
Acute appendicitis




Incisional hernia containing bowel and fluid

PITFALLSCASES

Is the resistive index measured correctly?
No- mirror image venous flow ismeasured as diastolic flow

Initial Bedside study
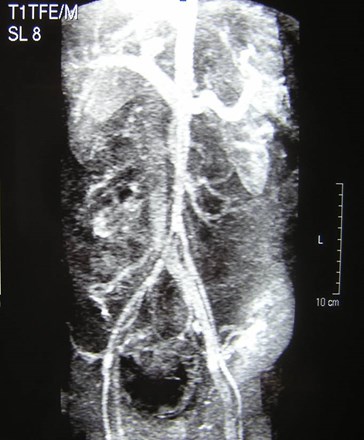
MRA MRV
EIA EIV

Follow Up Study
Pulsatile venous flow due to fluid overload,improves with medical therapy


Day 1


Day 2
Pain over transplant


Patient receives 2 pediatric transplants
5-2007
10-2007

Is this renal artery stenosis?

Normal arcuate waveforms- no parvus tardus flow
High RA velocities due to high flowrate through small vessel

BONUS CASES

Early post operative imagingin renal transplant with tworenal arteries


Iliac artery stenosis, proximal totransplant

Re-imaging post stent placement

Re-imaging 2 months later with elevated creatinine
U
M
L

Lower pole Doppler
Upper pole Doppler
Interlobar
arteries
Mainarteries

Stenosis of upper pole renal artery
Origin upper pole artery

Few days later
Initial post operative study
Torsion Renal Transplant

Initial study


Pre CT Post CT
US after detorsion

The End