|
|
Clostridium Difficile Colitis
Pseudomembranous Colitis
General Considerations
- Characterized by pseudomembrane, a yellowish-white plaque seen on the mucosa
- Usually involves colon, although small bowel can be involved
- Occurs primarily in hospitalized patients
- Almost 20% of hospitalized patients acquire C difficile during hospitalization
- Occurs in adults, especially the elderly, more often than children
- Almost always secondary to antibiotic therapy with overgrowth of Clostridium difficile, a gram-positive, anaerobic bacillus normally present in about 2-3 % of healthy adults
- Pseudomembranous colitis has also been described in
- Colonic obstruction
- Abdominal surgery
- Hypotension
- Lymphoma and leukemia
- Advanced HIV infection
- C difficile releases toxin A (enterotoxin) and toxin B (cytotoxin) which mediate endothelial damage in target cells, leading to
- Mucosal inflammation and injury
- Antibiotics most commonly associated with pseudomembranous colitis are almost always administered orally and may include any antibiotic, but especially
- Ampicillin
- Cephalosporins
- Clindamycin
- Lincomycin
Clinical Findings
- Begins within a few days to 6 weeks after antibiotic treatment
- Diarrhea
- Abdominal pain
- Anorexia and malaise
- Fever
- Leukocytosis
Imaging Findings
- Diagnosis is made by stool samples which reveal C difficile or its toxins or, more often, by colonoscopy
- Sigmoidoscopy alone may miss up to 10% of cases
- Conventional radiographs are insensitive but may show dilated colon, thumbprinting and thickening of the haustral folds
- CT
- The imaging study most often used to suggest diagnosis
- But same findings seen with pseudomembranous colitis can occur with other inflammatory and ischemic diseases
- Thickening of the wall of the colon, usually pan-colonic but can be focal
- Accordion sign
- Contrast trapped within very thick haustra produce alternating bands of high and low density
- Pericolonic stranding
- Usually mild compared to the bowel wall thickening
- Target sign
- Mucosal hyperemia from inflammation produces a central bulls-eye surrounded by less dense edematous bowel wall
- Ascites
- Usually only in severe cases
Differential Diagnosis
- Ischemic colitis
- Crohn disease
- Typhlitis
- Ulcerative colitis
- Diverticulitis
Treatment
- Stop antibiotics
- Most patients recover even without specific therapy
- If severe, vancomycin or metronidazole (Flagyl) can be used to treat the C difficile organism
Complications
- Relapse in up to 50% of cases
- Toxic megacolon and perforation
Prognosis
- Mortality rates are from 1-3.5%
- Morbidity rates are high
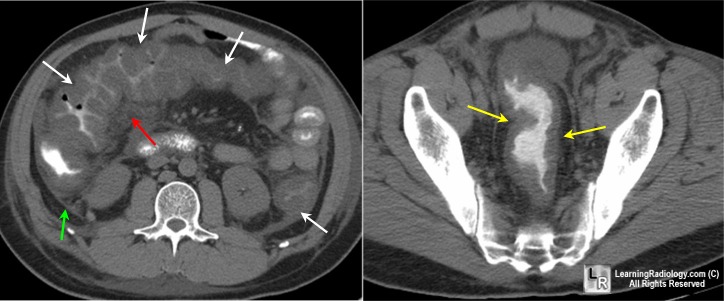
Pseudomembranous colitis. (Left) Axial CT scan of the midabdomen utilizing oral but not intravenous contrast demonstrates marked thickening of the colonic wall (white arrows) producing the so-called "accordion sign." There is a small amount of pericolonic stranding (red arrow) and ascites (green arrow). (Right) Axial CT scan through the pelvis shows marked thickening of the wall of the rectum (yellow arrows) indicating this is a pan-colitis..
For additional information about this disease, click on this icon if seen above.
For same photos without annotations, click here
eMedicine Pseudomembranous Colitis Author and Co-authors: Vinay K Gheyi, MD, MBBS; John S Wills, MD; Raul N Uppot, MD
|
|
|