|
|
Paget Disease
General Considerations
- Multifocal chronic skeletal disease due to chronic paramyxoviral infection
- Prevalence
- 3% of individuals >40 years
- 10% of persons >80 years
- Unusual <40 years
- M:F = 2:1
- Histology
- Increased resorption and increased bone formation
- Newly formed bone is abnormally soft with disorganized trabecular pattern
- Active or Osteolytic phase
- Aggressive bone resorption with lytic lesions
- Replacement of hematopoietic bone marrow by fibrous connective tissue with numerous large vascular channels
- Inactive or Quiescent phase
- Decreased bone turnover with skeletal sclerosis and thickening of the cortex
- Mixed pattern
- Lytic and sclerotic phases frequently coexist
Clinical findings
- Asymptomatic (1/5)
- When symptomatic, symptoms may include
- Fatigue
- Enlarged hat size
- Peripheral nerve compression
- Neurologic disorders from compression of brainstem (basilar invagination)
- Hearing loss, blindness
- Facial palsy (narrowing of neural foramina) - rare
- Pain from(a)primary disease process is rare so think of
- Pathologic fracture
- Malignant transformation
- Secondary degenerative joint disease aggravated by skeletal deformity
- High-output congestive heart failure from markedly increased perfusion (rare)
- Increased alkaline phosphatase (increased bone formation)
- Hydroxyproline increased (increased bone resorption)
- Normal serum calcium + phosphorus
Sites of involvement
- Usually polyostotic and asymmetric
- Pelvis (75%) most common, followed by
- Lumbar spine
- Thoracic spine
- Proximal femur
- Calvarium
- Scapula
- Distal femur
- Proximal tibia
- Proximal humerus
Imaging Findings
- Classical triad
- Thickening of the cortex
- Accentuation of the trabecular pattern
- Increased size of bone
- Cyst-like areas
- Skull (involvement in 29-65%)
- Inner and outer table involved
- Leads to diploic widening
- Osteoporosis circumscripta is well-defined lysis, most commonly in frontal bone producing well-defined geographic lytic lesion in skull
- Represents early destructive phase of disease active stage)
- "Cotton wool" appearance represents mixed lytic and blastic pattern of thickened calvarium (later stage)
- Basilar invagination with encroachment on foramen magnum
- Deossification and sclerosis in maxilla
- Sclerosis of skull base
- Long bones (almost invariably starts at end of bone)
- "Candle flame" or "blade of grass" pattern of lysis is the advancing tip of V-shaped lytic defect in diaphysis of long bone originating in subarticular site
- Lateral curvature of femur
- Anterior curvature of tibia (commonly resulting in fracture)
- Pelvis

- Thickened trabeculae in sacrum, ilium
- Rarefaction in central portion of ilium (looks like a large lytic lesion)
- Thickening of iliopectineal line
- Acetabular protrusio with secondary degenerative joint disease
- Spine (upper cervical, low dorsal, midlumbar most common sites)
- Coarse trabeculations at periphery of bone
- "Picture-frame vertebra" mimics bone-within-bone appearance
- Enlarged vertebral body with reinforced peripheral trabeculae and more lucent center, typically in lumbar spine
- "Ivory vertebra" is a blastic vertebra with increased density
- Ossification of spinal ligaments, paravertebral soft tissue, disk spaces can occur
Bone scan
- Sensitivity
- Scintigraphy and radiography (60%)
- Scintigraphy only (27%)
- Radiography only (13%)
- Usually markedly increased uptake (symptomatic lesions strikingly positive)
- Normal scan may occur in some burned-out lesions
- Marginal uptake can be seen in lytic lesions
Bone marrow scan
- Sulfur colloid bone marrow uptake is decreased (marrow replacement by cellular fibrovascular tissue)
MRI Findings
- Hypointense area / area of signal void on T1WI + T2WI (cortical thickening, coarse trabeculation)
- Widening of bone
- Reduction in size and signal intensity of medullary cavity due to replacement of high-signal-intensity fatty marrow by medullary bone formation
- Focal areas of higher signal intensity than fatty marrow (from cyst-like fat-filled marrow spaces)
- Areas of decreased signal intensity within marrow on T1WI and increased intensity on T2WI (= fibrovascular tissue resembling granulation tissue)
Complications
- Associated neoplasia (0.7-20%)
- Sarcomatous transformation into osteosarcoma (22-90%), fibrosarcoma /malignant fibrous histiocytoma (29-51%), chondrosarcoma (1-15%)
- Sarcomas are usually osteolytic in pelvis, femur, humerus
- Giant cell tumor occurs in 3-10%
- Lytic expansile lesion in skull, facial bones
- Lymphoma or plasma cell myeloma are reported
- Fracture
- "Banana fracture" = tiny horizontal cortical infractions (“Looser lines”)on convex surfaces of lower extremity long bones (lateral bowing of femur, anterior bowing of tibia)
- Compression fractures of vertebrae
- Early-onset osteoarthritis
Treatment
- Calcitonin, diphosphonate, mithramycin
- Detection of recurrence:
- In 1/3 detected by bone scan
- In 1/3 detected by biomarkers (alkaline phosphatase, urine hydroxyproline)
- In 1/3 by scan and biomarkers simultaneously
DDx
- Depends on the bone in which it occurs
- Skull
- Osteolytic or osteoblastic metastases
- Long bones
- Metastases

- Chronic osteomyelitis (thickened cortex)
- Old trauma (thickened cortex)
- Hodgkin’s disease
- Spine
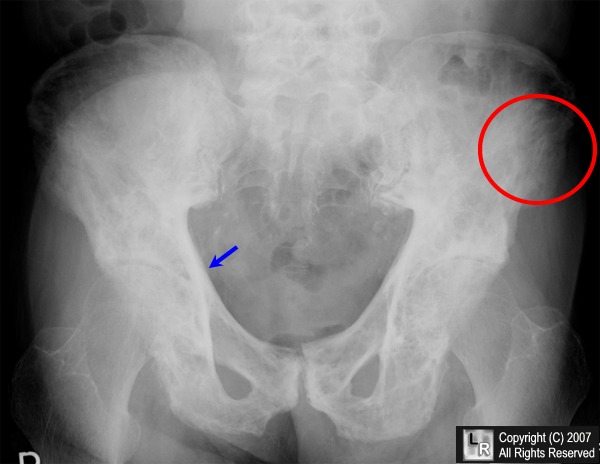
Paget's Disease -- pelvis. Frontal radiograph of the pelvis demonstrates the classical triad of thickening
of the cortex (blue arrow), accentuation of the trabecular pattern (red circle) and increased density of the bone.
For additional information about this disease, click on this icon above.
For this same photo without the arrows, click here
|
|
|